Official Do Not Resuscitate Order Template for Virginia State
The Virginia Do Not Resuscitate (DNR) Order form is a crucial document that allows individuals to express their wishes regarding medical treatment in the event of a life-threatening situation. This form is designed for patients who wish to forgo cardiopulmonary resuscitation (CPR) and other life-saving measures if their heart stops or they stop breathing. It is essential for ensuring that a person's preferences are respected during critical moments when they may not be able to communicate. The DNR Order must be completed and signed by a licensed physician, and it requires clear identification of the patient. Additionally, it is vital that the form be easily accessible to emergency medical personnel. By understanding the implications of this document, individuals can make informed decisions about their healthcare and end-of-life choices. Proper completion and adherence to the DNR Order can provide peace of mind for patients and their families during challenging times.
Misconceptions
Understanding the Virginia Do Not Resuscitate (DNR) Order form is crucial for making informed healthcare decisions. Here are five common misconceptions about the DNR form that need clarification:
- A DNR means no medical care at all. This is false. A DNR only prevents resuscitation efforts in the event of cardiac or respiratory arrest. Other medical treatments can still be provided.
- Only terminally ill patients can have a DNR. This is not true. Any patient, regardless of their health status, can request a DNR if they wish to avoid resuscitation.
- A DNR is a permanent decision. This misconception can lead to unnecessary worry. A DNR can be revoked or changed at any time by the patient or their legal representative.
- Healthcare providers must follow a DNR order in all situations. This is misleading. A DNR order is only applicable in specific circumstances, such as when the patient is in cardiac or respiratory arrest.
- A DNR is the same as a living will. This is incorrect. While both documents relate to end-of-life care, a DNR specifically addresses resuscitation efforts, whereas a living will outlines broader healthcare preferences.
It is essential to have open discussions with healthcare providers about the DNR order and its implications. This ensures that your wishes are understood and respected.
Virginia Do Not Resuscitate Order: Usage Instruction
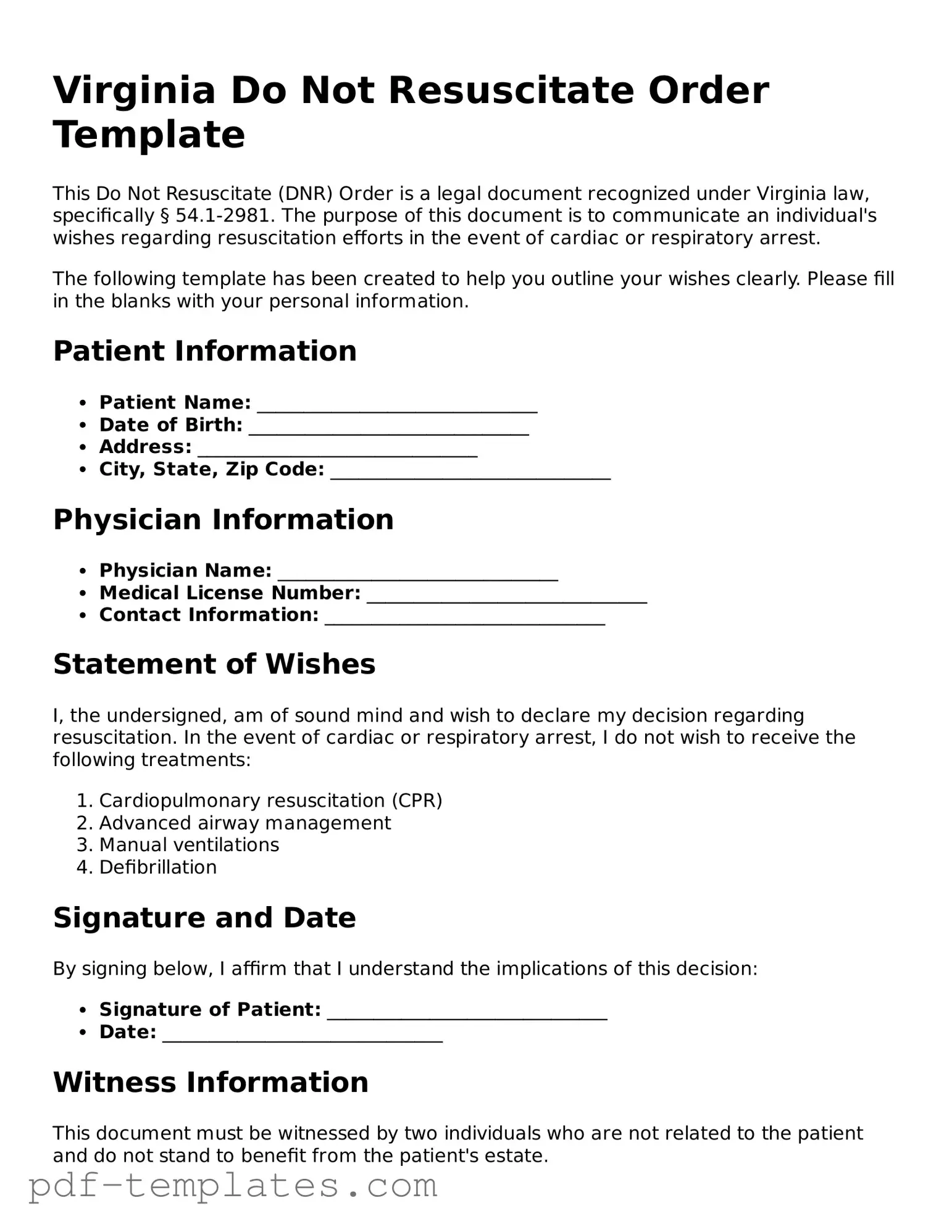
Filling out the Virginia Do Not Resuscitate Order form is a straightforward process that ensures your healthcare preferences are known and respected. This form is important for communicating your wishes regarding medical treatment in emergency situations. Follow these steps carefully to complete the form accurately.
- Obtain the Virginia Do Not Resuscitate Order form. You can find it online or request a copy from your healthcare provider.
- Read the instructions provided with the form to understand its purpose and implications.
- Fill in your full name, date of birth, and address at the top of the form.
- Designate a healthcare representative by providing their name and contact information. This person will help ensure your wishes are followed.
- Clearly indicate your decision regarding resuscitation by checking the appropriate box. Make sure to review your choice carefully.
- Sign and date the form in the designated area. Your signature is necessary to validate your wishes.
- Have the form witnessed. Virginia law requires that at least two witnesses sign the form, confirming they saw you sign it.
- Make copies of the completed form. Keep one for your records and provide copies to your healthcare provider and your designated representative.
- Discuss your wishes with your family and healthcare team to ensure everyone is informed and understands your decisions.
Once you have completed the form, it is essential to communicate your wishes with those involved in your care. This ensures that your preferences are honored in any medical situation. Keep the form accessible, and remember to review it periodically, especially if your circumstances change.
Common mistakes
-
Not including the patient's full name. Ensure the name is accurate and matches official identification.
-
Failing to sign the form. A signature is necessary for the order to be valid.
-
Not dating the form. Always include the date when the form is completed to establish its validity.
-
Using unclear language. Be specific about the patient's wishes to avoid confusion.
-
Not discussing the order with healthcare providers. Communication with doctors is crucial for understanding the implications.
-
Forgetting to update the form. Changes in the patient's condition or wishes should be reflected in a new form.
-
Neglecting to involve family members. Family input can provide support and clarity regarding the patient's wishes.
-
Not keeping copies of the form. Always retain a copy for personal records and share it with healthcare providers.
-
Ignoring state-specific requirements. Each state may have unique rules that must be followed.
-
Assuming verbal agreements are enough. Written documentation is necessary to ensure the patient's wishes are honored.
PDF Features
| Fact Name | Description |
|---|---|
| Definition | A Virginia Do Not Resuscitate (DNR) Order is a medical order that instructs healthcare providers not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. |
| Governing Law | The DNR Order in Virginia is governed by the Virginia Code § 54.1-2982. |
| Eligibility | Any adult, or a legally authorized representative of a minor, can complete a DNR Order in Virginia. |
| Form Requirements | The DNR Order must be signed by a physician and the patient or their authorized representative. |
| Validity | A DNR Order is valid throughout Virginia once properly completed and signed. |
| Emergency Medical Services | Emergency medical services personnel are required to honor a valid DNR Order when they encounter it. |
| Revocation | A DNR Order can be revoked at any time by the patient or their authorized representative. |
| Notification | It is advisable to inform family members and healthcare providers of the existence of a DNR Order. |
| Documentation | Healthcare facilities should maintain a copy of the DNR Order in the patient’s medical record. |
| Advance Directives | A DNR Order is often part of a broader advance directive, which outlines a person's healthcare preferences. |
Dos and Don'ts
When filling out the Virginia Do Not Resuscitate Order form, it’s important to follow specific guidelines to ensure your wishes are clearly communicated. Here’s a list of things you should and shouldn’t do:
- Do discuss your wishes with your healthcare provider.
- Do ensure that the form is signed by you and a witness.
- Do keep a copy of the completed form for your records.
- Do inform your family members about your decision.
- Don't leave any sections of the form blank.
- Don't assume that verbal instructions are enough.
- Don't forget to update the form if your wishes change.
- Don't neglect to review the form regularly.
Similar forms
The Virginia Do Not Resuscitate (DNR) Order form shares similarities with the Advance Directive. Both documents serve as legal instruments that communicate an individual’s healthcare preferences when they are unable to speak for themselves. An Advance Directive typically includes instructions regarding medical treatment and appoints a healthcare proxy, while the DNR specifically addresses the individual's wishes regarding resuscitation efforts. Together, they ensure that a person's end-of-life choices are respected and followed by healthcare providers.
As individuals navigate their healthcare choices, understanding the various forms available is essential. Among these, the California Independent Contractor Agreement plays a significant role in defining the relationship between contractors and clients, ensuring clear communication and compliance with state laws. For those looking for comprehensive documents to support their needs, All California Forms provides a valuable resource.
Another document that aligns closely with the Virginia DNR is the Physician Orders for Life-Sustaining Treatment (POLST). The POLST form is designed for patients with serious illnesses or those nearing the end of life. Like the DNR, it provides clear medical orders regarding resuscitation and other life-sustaining treatments. The POLST form is more comprehensive, detailing a wider range of medical interventions, while the DNR focuses solely on resuscitation preferences.
The Medical Power of Attorney is another relevant document. This legal tool allows individuals to appoint someone to make healthcare decisions on their behalf if they become incapacitated. While the DNR specifies what should not be done in terms of resuscitation, the Medical Power of Attorney empowers a designated individual to interpret and make choices based on the patient's overall wishes, including whether to initiate resuscitation.
Living Wills also bear resemblance to the Virginia DNR. A Living Will is a type of Advance Directive that outlines an individual’s preferences for medical treatment in situations where they cannot communicate. It often includes decisions about resuscitation, thus overlapping with the DNR. While the DNR specifically addresses resuscitation, the Living Will may cover a broader spectrum of medical interventions, emphasizing the individual's overall treatment preferences.
The Do Not Intubate (DNI) order is another document that parallels the DNR. A DNI specifically instructs healthcare providers not to place a breathing tube in a patient who is unable to breathe on their own. While the DNR focuses on not performing cardiopulmonary resuscitation (CPR), the DNI addresses a different aspect of life-sustaining treatment, providing clarity on the patient’s wishes regarding respiratory support.
The Comfort Care Order is also similar in nature. This document emphasizes providing comfort and alleviating suffering rather than prolonging life through aggressive medical interventions. While the DNR prohibits resuscitation efforts, the Comfort Care Order focuses on ensuring that patients receive palliative care, which may include pain management and other supportive measures without aggressive life-sustaining treatments.
Finally, the Health Care Proxy form is akin to the Virginia DNR in that it designates a person to make healthcare decisions on behalf of the individual. While the DNR outlines specific preferences regarding resuscitation, the Health Care Proxy allows the appointed individual to make decisions based on the patient’s values and wishes, which may include considerations about resuscitation in various medical scenarios.
Check out Popular Do Not Resuscitate Order Forms for Different States
Texas Dnr Form - A DNR order must be signed by a patient or their authorized representative and a physician.
Dnr Document - The DNR order may specify particular conditions under which it applies.
For individuals wishing to clarify their medical treatment preferences, the form titled "Texas Do Not Resuscitate Order Process" provides vital guidance on how to complete and present a DNR order legally. To learn more about this important document, visit the Texas Do Not Resuscitate Order form.
Polst Form Wa - A Do Not Resuscitate Order indicates a wish not to receive CPR in the event of cardiac arrest.
Pennsylvania Dnr - An essential form for anyone wanting to avoid invasive treatments that prolong dying rather than living.