Do Not Resuscitate Order Document
The Do Not Resuscitate (DNR) Order form plays a crucial role in healthcare decision-making, particularly for individuals facing serious medical conditions. This document allows patients to express their wishes regarding resuscitation efforts in the event of cardiac arrest or respiratory failure. It is essential for ensuring that a person's preferences are respected during critical moments when they may be unable to communicate. Typically, the form must be completed and signed by a physician, ensuring that it meets the legal requirements for validity. It is important to note that a DNR order does not affect other aspects of medical care; patients will continue to receive necessary treatments and comfort measures. Understanding the nuances of this form can empower individuals and families to make informed decisions about end-of-life care, aligning medical interventions with personal values and desires.
Misconceptions
Understanding the Do Not Resuscitate (DNR) Order form is crucial for patients and their families. Misconceptions can lead to confusion and anxiety during critical times. Here are seven common misconceptions:
-
A DNR means no medical care at all.
This is incorrect. A DNR specifically addresses resuscitation efforts during cardiac arrest. Patients can still receive other medical treatments and interventions.
-
Only terminally ill patients need a DNR.
While many people with terminal conditions choose a DNR, it is not limited to them. Anyone can request a DNR based on their personal healthcare wishes.
-
A DNR is the same as euthanasia.
This misconception is significant. A DNR does not allow for the active ending of life. It simply means that a patient does not wish to undergo resuscitation efforts.
-
Once a DNR is in place, it cannot be changed.
This is false. Patients or their legal representatives can revoke or modify a DNR at any time, as long as they are competent to do so.
-
A DNR is only valid in hospitals.
A DNR can be valid in various settings, including at home or in nursing facilities, as long as the appropriate documentation is present and recognized.
-
Healthcare providers must follow a DNR order without question.
Healthcare providers are obligated to respect DNR orders, but they must also ensure that the order is valid and properly documented. They may seek clarification if needed.
-
Having a DNR means giving up hope.
This is a harmful misconception. A DNR reflects a patient's values and preferences regarding end-of-life care, and it does not equate to a lack of hope for recovery.
Clarifying these misconceptions can help ensure that patients and families make informed decisions regarding their healthcare preferences.
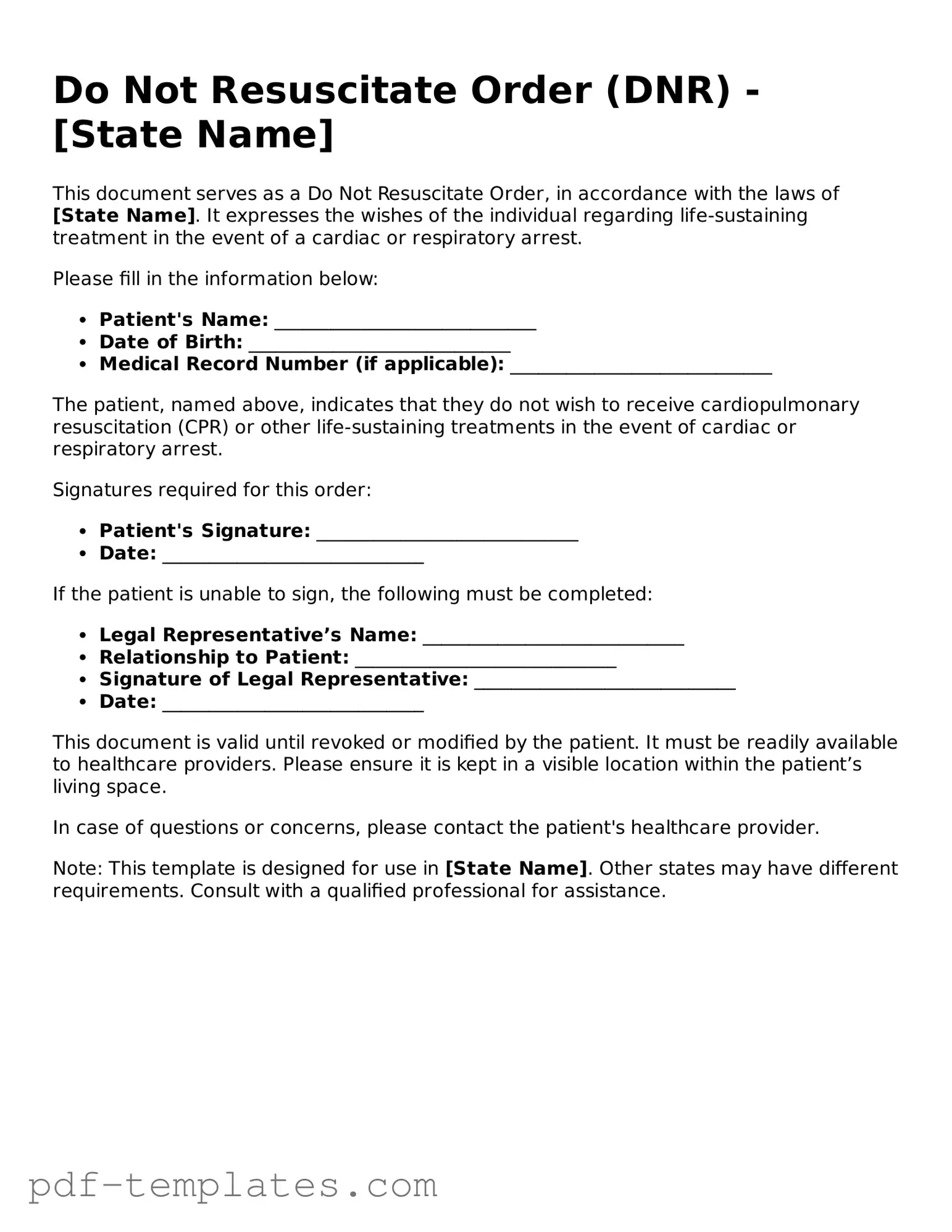
Do Not Resuscitate Order - Customized for State
Do Not Resuscitate Order: Usage Instruction
Completing a Do Not Resuscitate Order (DNR) form is an important step for individuals who wish to express their preferences regarding medical treatment in emergency situations. The following steps provide a clear guide to filling out the form accurately.
- Obtain the DNR form from a healthcare provider or relevant medical authority.
- Carefully read the instructions included with the form.
- Fill in your full name and date of birth in the designated fields.
- Provide the name of your healthcare provider, including their contact information.
- Indicate your preferences regarding resuscitation by checking the appropriate boxes.
- Sign and date the form to validate your choices.
- Have a witness sign the form if required, ensuring they also date it.
- Make copies of the completed form for your records and for your healthcare provider.
- Discuss your DNR order with your family and healthcare team to ensure everyone is informed.
Common mistakes
-
Failing to clearly indicate the patient's wishes. It is crucial to ensure that the Do Not Resuscitate (DNR) order accurately reflects the patient's desires regarding resuscitation efforts.
-
Not signing the form. A DNR order is not valid unless it is signed by the patient or their authorized representative. Always double-check that the signature is present.
-
Using outdated forms. Medical practices may update their forms regularly. Using an old version can lead to confusion and potential legal issues.
-
Not involving healthcare providers. It is advisable to discuss the DNR order with a healthcare professional to ensure it aligns with medical standards and the patient's health condition.
-
Overlooking witness requirements. Some states require a witness to sign the DNR order. Not following these requirements can invalidate the document.
-
Neglecting to review and update the order. Life circumstances can change, and it’s important to regularly revisit the DNR order to ensure it still reflects the patient's wishes.
-
Not providing copies to relevant parties. After completing the DNR order, copies should be distributed to healthcare providers, family members, and anyone involved in the patient's care.
-
Misunderstanding the scope of the DNR order. Some people mistakenly believe that a DNR means no medical care at all. It is essential to clarify that it specifically pertains to resuscitation efforts.
-
Failing to communicate with family members. Open discussions about the DNR order with family can prevent misunderstandings and ensure everyone is on the same page regarding the patient's wishes.
PDF Features
| Fact Name | Description |
|---|---|
| Definition | A Do Not Resuscitate (DNR) Order is a legal document that instructs medical personnel not to perform cardiopulmonary resuscitation (CPR) in the event of cardiac arrest. |
| Legal Authority | In the United States, DNR Orders are governed by state laws, which vary widely. For example, in California, the governing law is the California Health and Safety Code Section 4780. |
| Patient Autonomy | A DNR Order respects the patient's wishes regarding end-of-life care, allowing individuals to make decisions about their medical treatment in advance. |
| Signature Requirements | Most states require a DNR Order to be signed by a physician and the patient or their legal representative to be considered valid. |
| Emergency Medical Services | Emergency medical services (EMS) personnel are trained to recognize DNR Orders and must follow them unless they are not properly documented. |
| Revocation | A DNR Order can be revoked at any time by the patient or their legal representative, and this must be clearly communicated to healthcare providers. |
Dos and Don'ts
When filling out a Do Not Resuscitate (DNR) Order form, it's important to approach the task with care and consideration. Here are some guidelines to help you navigate this process effectively.
- Do ensure that you understand the implications of a DNR order. It is crucial to know what it means for your medical care.
- Do discuss your wishes with your healthcare provider. Open communication can clarify your options and ensure your preferences are respected.
- Do involve family members or loved ones in the conversation. Their support can be invaluable, and they should be aware of your decisions.
- Do complete the form accurately. Double-check all information to avoid any potential confusion in an emergency.
- Don't rush the process. Take your time to consider your choices and the potential outcomes.
- Don't assume that a verbal agreement is sufficient. Written documentation is necessary for a DNR order to be recognized by medical personnel.
- Don't neglect to review and update your DNR order as needed. Your preferences may change over time, and it's important to keep your documents current.
Similar forms
A Living Will is a document that outlines an individual’s wishes regarding medical treatment in the event they become unable to communicate. Like a Do Not Resuscitate Order (DNR), it provides guidance to healthcare providers about what actions to take or avoid. Both documents focus on personal preferences for end-of-life care, ensuring that medical interventions align with the individual’s values and desires.
A Healthcare Proxy, also known as a Durable Power of Attorney for Healthcare, allows a person to designate someone else to make medical decisions on their behalf. Similar to a DNR, it emphasizes the importance of respecting a person's wishes regarding medical treatment. While a DNR specifically addresses resuscitation efforts, a Healthcare Proxy can cover a broader range of medical decisions, ensuring that an individual’s preferences are honored even if they cannot speak for themselves.
An Advance Directive is a comprehensive document that combines elements of both a Living Will and a Healthcare Proxy. It allows individuals to express their wishes for medical treatment and appoint someone to make decisions for them. Like a DNR, an Advance Directive serves to communicate a person’s values and preferences, helping healthcare providers understand what care is desired or refused in critical situations.
The Physician Orders for Life-Sustaining Treatment (POLST) form is another important document. It translates a patient’s wishes regarding life-sustaining treatments into actionable medical orders. Similar to a DNR, the POLST form is intended for individuals with serious illnesses or those who are nearing the end of life. It ensures that healthcare providers are aware of and respect the patient’s treatment preferences, particularly in emergency situations.
A Do Not Intubate (DNI) order is closely related to a DNR. While a DNR focuses on not performing cardiopulmonary resuscitation, a DNI specifically addresses the use of mechanical ventilation. Both documents express a patient’s desire to avoid certain aggressive medical interventions. They serve to clarify preferences in critical care scenarios, allowing individuals to maintain control over their medical treatment.
In addressing the critical aspects of emergency preparedness, it is essential for Californians to be informed about various resources available, including the All California Forms which provide vital information on insurance coverage options against earthquake damage, thereby reinforcing the significance of being ready for potential seismic events in the state.
Finally, a Mental Health Advance Directive allows individuals to outline their preferences for mental health treatment in case they become unable to make decisions. Like a DNR, it is designed to communicate specific wishes to healthcare providers. This document ensures that a person’s values and preferences regarding mental health care are respected, similar to how a DNR communicates preferences for physical health interventions.
More Documents
What to Include in a Letter of Recommendation - An assessment of the candidate's time management and organizational skills.
The Asurion F-017-08 MEN form is designed to streamline the process of submitting insurance claims for electronic devices, allowing customers to quickly access the support they require. To understand more about this essential document and to initiate your claim, you can visit https://pdftemplates.info/asurion-f-017-08-men-form/ and follow the necessary steps.
Prescription Bottle Label Requirements - The label may provide warnings regarding the medication's use.