Get Cna Shower Sheets Form in PDF
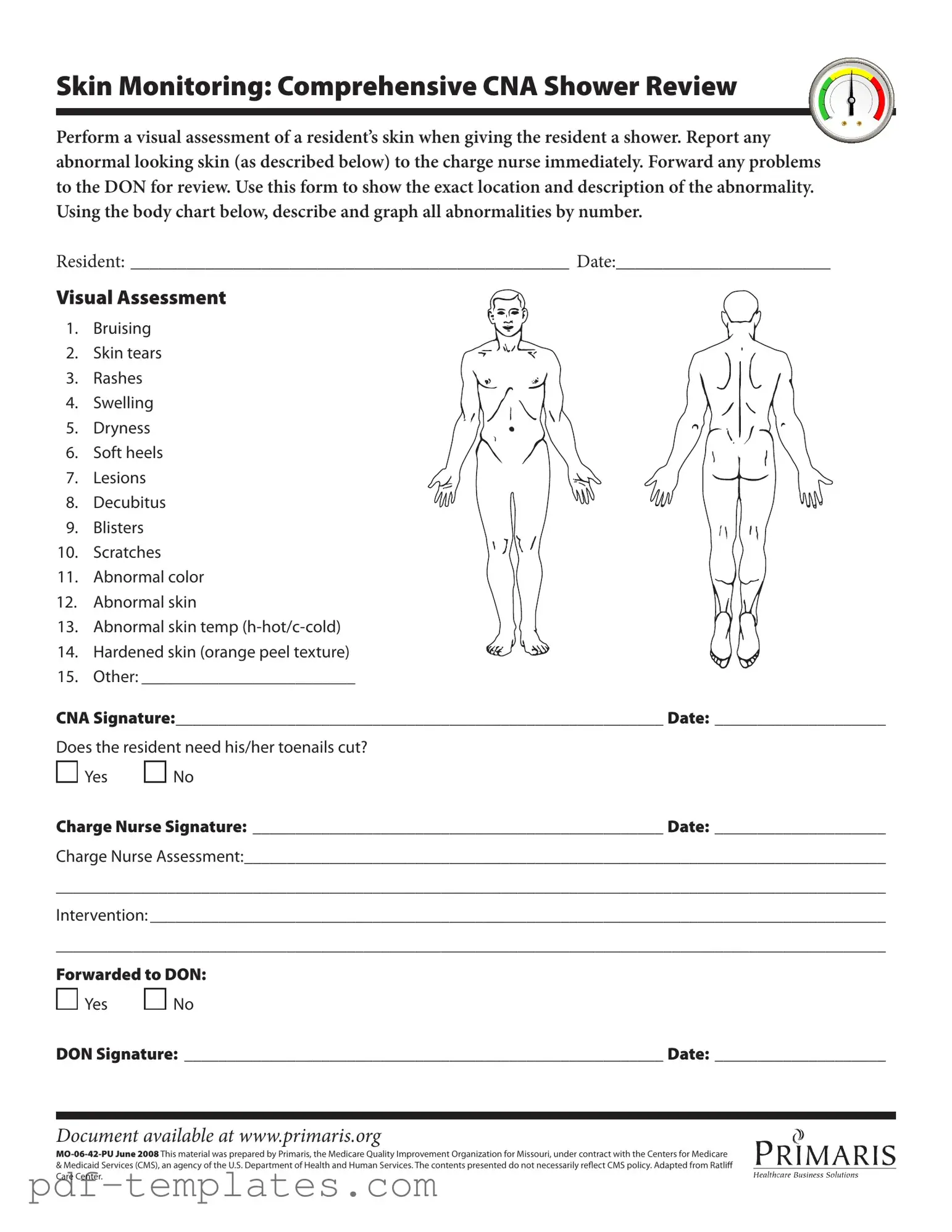
The CNA Shower Sheets form plays a crucial role in ensuring the health and safety of residents during personal care activities, particularly showers. This form serves as a tool for Certified Nursing Assistants (CNAs) to conduct a thorough visual assessment of a resident’s skin condition while providing bathing assistance. It outlines specific abnormalities that CNAs must look for, including bruising, skin tears, rashes, and signs of infection. By documenting these findings, CNAs can communicate effectively with charge nurses and the Director of Nursing (DON) regarding any concerns that arise. The form includes a body chart for precise location mapping of any abnormalities, which enhances clarity in reporting. Additionally, it prompts CNAs to assess other aspects of care, such as whether a resident requires toenail trimming. The signatures of both the CNA and the charge nurse are essential for accountability and continuity of care. This process not only fosters a proactive approach to skin health but also aligns with regulatory standards set forth by healthcare authorities.
Misconceptions
Understanding the CNA Shower Sheets form is essential for ensuring proper skin monitoring and care for residents. However, several misconceptions often arise regarding its use and purpose. Here are nine common misunderstandings:
- The form is only for documenting severe skin issues. Many believe that the CNA Shower Sheets are only necessary for serious conditions like decubitus ulcers. In reality, the form is designed to document a range of skin conditions, from minor abrasions to significant abnormalities.
- Only licensed nurses can fill out the form. Some think that only registered nurses or licensed practical nurses are authorized to complete this form. However, certified nursing assistants (CNAs) play a crucial role in the initial assessment and can fill it out based on their observations.
- Skin monitoring is optional during showers. There is a misconception that skin monitoring is not mandatory during showering. In fact, it is a critical part of resident care that must be performed consistently to ensure any changes are promptly addressed.
- The form does not require detailed descriptions. Some may believe that a simple notation is sufficient. The form actually emphasizes the importance of detailed descriptions and accurate locations of any abnormalities to aid in effective communication with nursing staff.
- All skin conditions require immediate intervention. While it is vital to report any abnormalities, not all conditions necessitate immediate action. Some issues may require monitoring rather than urgent intervention, and the charge nurse will determine the appropriate response.
- Only the charge nurse reviews the form. There is a belief that the charge nurse is the only one who reviews the completed form. In fact, the Director of Nursing (DON) also plays a role in reviewing the information for ongoing care and quality assurance.
- Documentation is not important if the issue is minor. Many think that if an issue seems minor, it doesn’t need to be documented. However, thorough documentation is crucial for tracking changes over time and ensuring comprehensive care.
- The form is only relevant for elderly residents. Some individuals assume that the CNA Shower Sheets are applicable only to elderly residents. This form is relevant for all residents requiring assistance with personal care, regardless of age.
- Once submitted, the form is forgotten. There is a misconception that after the form is submitted, it is no longer referenced. In truth, the information collected is vital for ongoing assessments and care plans, and it remains an integral part of the resident's health record.
By addressing these misconceptions, caregivers can better understand the importance of the CNA Shower Sheets form and its role in promoting the health and well-being of residents.
Cna Shower Sheets: Usage Instruction
Completing the CNA Shower Sheets form is essential for documenting skin assessments during resident showers. This process ensures that any abnormalities are promptly reported and addressed. Follow these steps to accurately fill out the form.
- Begin by writing the resident's name in the designated space labeled RESIDENT:.
- Fill in the current date next to DATE:.
- Conduct a visual assessment of the resident's skin during the shower.
- Identify any abnormalities from the provided list, which includes bruising, skin tears, rashes, and more.
- Use the body chart included in the form to indicate the location of each abnormality by number.
- In the space provided for Other:, describe any additional abnormalities not listed.
- Sign the form in the section labeled CNA Signature: and include the date.
- Indicate whether the resident needs a toenail cut by selecting Yes or No.
- Have the charge nurse sign the form in the Charge Nurse Signature: section and include the date.
- In the Charge Nurse Assessment: section, provide a brief summary of the findings.
- Document any interventions taken in the Intervention: section.
- Note whether the report has been forwarded to the Director of Nursing (DON) by marking Yes or No.
- Finally, have the DON sign the form in the DON Signature: section and include the date.
Common mistakes
When filling out the CNA Shower Sheets form, individuals may encounter several common mistakes. Awareness of these errors can enhance the accuracy and effectiveness of the documentation process. Below is a list of eight frequent mistakes:
- Failure to perform a thorough visual assessment of the resident's skin before documenting findings.
- Neglecting to report abnormal skin conditions to the charge nurse immediately, which can delay necessary interventions.
- Inaccurate or incomplete descriptions of skin abnormalities, leading to confusion during follow-up assessments.
- Omitting the use of the body chart to graphically represent the location of abnormalities, which is crucial for clarity.
- Not signing and dating the form, which is essential for maintaining a proper record of care.
- Forgetting to indicate whether the resident needs toenail care, which is an important aspect of personal hygiene.
- Leaving the charge nurse assessment section blank or incomplete, which can hinder communication between staff members.
- Failing to forward the form to the Director of Nursing (DON) when necessary, potentially compromising the resident's care.
By addressing these mistakes, caregivers can ensure that the CNA Shower Sheets form is filled out correctly, ultimately benefiting the residents they serve.
File Specifics
| Fact Name | Details |
|---|---|
| Purpose | The CNA Shower Sheets form is used for documenting skin assessments during resident showers. |
| Skin Monitoring | CNA must perform a visual assessment of the resident’s skin and report any abnormalities to the charge nurse immediately. |
| Abnormalities | The form lists 15 types of skin abnormalities, including bruising, rashes, and lesions. |
| Documentation | Details about the location and description of any skin issues must be recorded on the form. |
| Signatures Required | The form requires signatures from the CNA, charge nurse, and, if necessary, the Director of Nursing (DON). |
| State-Specific Use | This form is used in Missouri and is governed by regulations from the Centers for Medicare & Medicaid Services (CMS). |
| Availability | The form can be accessed online at www.primaris.org. |
Dos and Don'ts
When filling out the CNA Shower Sheets form, it is essential to follow specific guidelines to ensure accurate documentation and effective communication with the healthcare team. Here are seven important do's and don'ts:
- Do perform a thorough visual assessment of the resident's skin during the shower.
- Do report any abnormalities immediately to the charge nurse.
- Do accurately describe and graph all abnormalities on the body chart provided.
- Do ensure that the resident's name and date are clearly filled out at the top of the form.
- Don't overlook any signs of skin issues, such as bruising or rashes.
- Don't forget to document whether the resident needs toenail care.
- Don't leave the form incomplete; ensure all sections are filled out before submitting.
Similar forms
The CNA Shower Sheets form shares similarities with the Incident Report form. Both documents are used to document and report unusual occurrences related to a resident's health. The Incident Report focuses on any incidents that may occur during care, while the CNA Shower Sheets specifically address skin abnormalities observed during showers. Both forms require signatures from staff members to verify the information and ensure accountability.
Another similar document is the Skin Assessment Form. This form is designed to monitor a resident’s skin condition over time. Like the CNA Shower Sheets, it includes specific criteria for assessing skin health, such as bruising, rashes, and lesions. Both documents aim to provide a clear and concise record of skin-related observations, helping to ensure timely interventions when necessary.
The Care Plan is also comparable to the CNA Shower Sheets. Care Plans outline the overall approach to a resident's care, including specific interventions for skin issues. While the CNA Shower Sheets focus on immediate observations during showers, the Care Plan provides a broader context for ongoing care, ensuring that skin monitoring is integrated into the resident's overall health strategy.
Understanding the significance of proper documentation in healthcare, it is essential to have forms that serve distinct purposes while ensuring comprehensive care. For instance, the https://formcalifornia.com/ provides a useful framework for designating financial decision-making powers, similar to how various forms in the healthcare sector address specific monitoring and reporting needs.
Similarly, the Daily Progress Notes serve a related purpose. These notes are used to track a resident’s condition and any changes that occur throughout the day. Just as the CNA Shower Sheets document specific skin assessments, Daily Progress Notes capture a variety of health observations, allowing for a comprehensive view of the resident's well-being.
The Wound Care Assessment form is another document that aligns closely with the CNA Shower Sheets. This form is specifically designed to evaluate and document wounds, including their size, appearance, and healing progress. Both forms emphasize the importance of visual assessments and require detailed descriptions to ensure proper care and follow-up.
The Medication Administration Record (MAR) also shares similarities. While the MAR focuses on the medications administered to a resident, it often includes notes on any side effects or reactions observed during administration. Like the CNA Shower Sheets, the MAR is crucial for maintaining accurate records and ensuring that any health changes are documented and addressed promptly.
The Resident Assessment Instrument (RAI) is another comparable document. The RAI is used to evaluate a resident's overall health and care needs, including skin assessments. While the CNA Shower Sheets provide a snapshot of skin condition during showers, the RAI offers a more comprehensive evaluation, helping to inform care strategies and interventions.
Lastly, the Quality Assurance and Performance Improvement (QAPI) plan is relevant. This document outlines the processes for monitoring and improving care quality within a facility. Like the CNA Shower Sheets, the QAPI plan emphasizes the importance of identifying and addressing issues related to resident care, including skin health, to enhance overall quality and safety in the care environment.
Other PDF Forms
Form Dr-835 - The form that grants access to tax records for a chosen representative.
To facilitate the sale process, it is recommended to use a reliable template, such as that found at All Florida Forms, which provides a comprehensive framework to create a properly formatted Florida Boat Bill of Sale.
Texas Hub Certification - Simplifies the task of overseeing and managing interest assignments.
What Is the Normal Range of Hiv Test - Clients must sign the form to acknowledge their test result and understanding of the information provided.