Official Do Not Resuscitate Order Template for California State
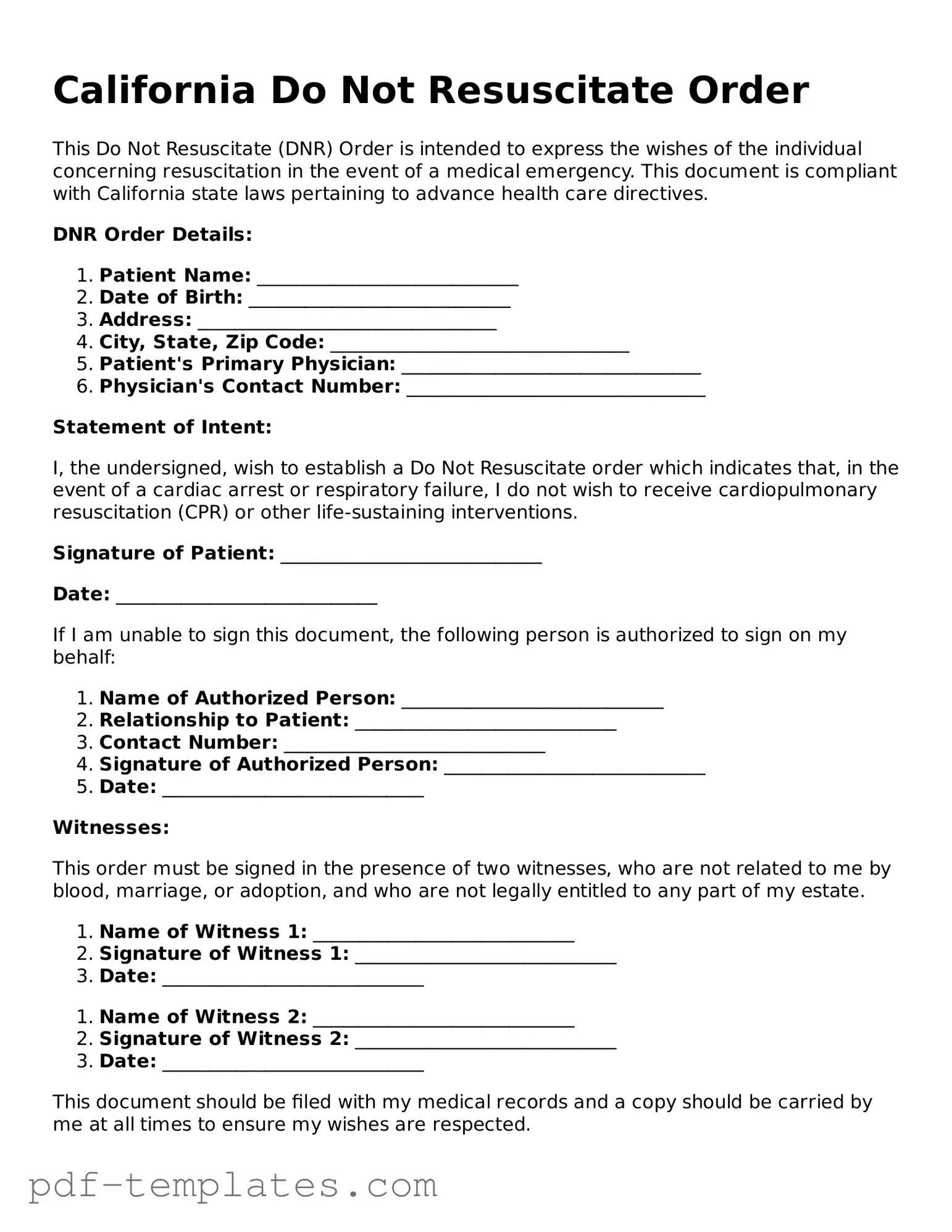
The California Do Not Resuscitate (DNR) Order form serves as a critical document for individuals wishing to express their preferences regarding medical treatment in emergency situations. This form is especially significant for those with serious medical conditions or terminal illnesses who wish to avoid aggressive resuscitation efforts, such as cardiopulmonary resuscitation (CPR), in the event of cardiac arrest or respiratory failure. It is essential that the form is completed accurately and signed by both the patient and their physician to ensure its validity. The DNR Order is designed to be easily recognizable and must be presented in a specific format, which includes clear language about the patient's wishes. Additionally, individuals can discuss their preferences with family members and healthcare providers to ensure everyone is informed and in agreement. Understanding the implications of a DNR Order can empower patients to make informed choices about their end-of-life care, providing peace of mind for both them and their loved ones.
Misconceptions
Misconceptions about the California Do Not Resuscitate (DNR) Order form can lead to confusion and misinformed decisions. Below are nine common misconceptions clarified for better understanding.
- A DNR means no medical care at all. Many people believe that a DNR order implies a complete withdrawal of all medical treatment. In reality, a DNR specifically addresses resuscitation efforts during cardiac or respiratory arrest but does not affect other medical care.
- A DNR is only for terminally ill patients. While many individuals with terminal conditions may choose to have a DNR, anyone can request one regardless of their health status. It is a personal choice based on individual values and preferences.
- A DNR is permanent and cannot be changed. A DNR order can be revoked or modified at any time by the patient or their legal representative. It is essential to communicate any changes to healthcare providers.
- Healthcare providers must follow a DNR order in all situations. A DNR order is only applicable in specific emergency situations. In cases where the patient is not in immediate danger, healthcare providers will still provide necessary medical treatment.
- A DNR must be signed by a physician. While a physician's signature is required for the DNR to be valid, patients can initiate the process themselves. They should discuss their wishes with their healthcare provider.
- A DNR is the same as an advance directive. Although both documents relate to end-of-life care, they serve different purposes. An advance directive outlines a person's wishes regarding various medical treatments, while a DNR specifically addresses resuscitation.
- Once a DNR is in place, it can’t be discussed. Open discussions about a DNR order are encouraged. Patients should feel comfortable talking about their wishes with family members and healthcare providers to ensure understanding and respect for their choices.
- Having a DNR means I will die alone. Many people fear that having a DNR will result in inadequate care or abandonment. In fact, healthcare providers are committed to providing compassionate care and support, regardless of a DNR status.
- A DNR is only for older adults. This misconception overlooks the fact that individuals of any age can choose to have a DNR order. Young people with serious health conditions may also opt for a DNR based on their personal values and circumstances.
Understanding these misconceptions can help individuals make informed decisions about their healthcare preferences and ensure their wishes are respected in critical situations.
California Do Not Resuscitate Order: Usage Instruction
Filling out the California Do Not Resuscitate Order form is an important step in ensuring your healthcare preferences are respected. Once you have completed the form, it is advisable to keep a copy for your records and share it with your healthcare providers and loved ones. This way, everyone is aware of your wishes.
- Obtain the California Do Not Resuscitate Order form. You can find it online or request it from your healthcare provider.
- Begin by filling in your personal information at the top of the form. This includes your full name, date of birth, and address.
- Next, indicate whether you are an adult or a minor. If you are filling out the form for a minor, ensure you have the necessary authority to do so.
- Clearly state your wishes regarding resuscitation. There will be specific sections where you can indicate your preferences.
- Sign and date the form. Your signature confirms that you understand the contents of the form and are making this decision voluntarily.
- Have the form witnessed. California law requires that you have at least one witness sign the form to validate it. The witness should not be a family member or someone who will benefit from your estate.
- Make copies of the completed form. Keep one for yourself and provide copies to your healthcare provider and any family members involved in your care.
Common mistakes
-
Not Understanding the Form's Purpose: Many individuals fill out the California Do Not Resuscitate Order form without fully grasping its implications. This form is a legal document that instructs medical personnel not to perform CPR in the event of cardiac arrest. It’s crucial to understand that this decision impacts emergency medical treatment.
-
Incorrectly Identifying the Patient: It’s common for people to mistakenly fill out the form with the wrong patient’s information. Ensure that the name, date of birth, and other identifying details are accurate. Errors in this section can lead to confusion during critical moments.
-
Failing to Sign and Date: A frequent oversight is neglecting to sign and date the form. Without a signature, the document is not valid. Make sure to include both the date and your signature to ensure the order is recognized by medical personnel.
-
Not Discussing the Decision with Family: Some individuals complete the form without consulting family members. It’s important to have conversations about end-of-life wishes. Family members should be aware of the decision to avoid confusion and potential disputes later on.
-
Not Keeping Copies Accessible: After filling out the form, people often forget to make copies. Keep several copies on hand. Share them with your healthcare provider, family members, and anyone who may need to reference the order in an emergency.
PDF Features
| Fact Name | Description |
|---|---|
| Definition | A California Do Not Resuscitate (DNR) Order is a medical order that indicates a person's wish not to receive cardiopulmonary resuscitation (CPR) in the event of cardiac or respiratory arrest. |
| Governing Law | The California DNR Order is governed by the California Health and Safety Code, Section 7180-7190. |
| Eligibility | Any adult who is capable of making healthcare decisions can complete a DNR Order. This includes individuals with terminal illnesses or severe medical conditions. |
| Form Requirements | The DNR Order must be signed by the patient or their legally authorized representative and a physician to be valid. |
| Placement | The completed DNR Order should be placed in a location that is easily accessible to emergency medical personnel, such as on the refrigerator or with the patient’s medical records. |
| Revocation | A DNR Order can be revoked at any time by the patient or their representative. This can be done verbally or in writing. |
| Emergency Services | Emergency medical personnel are required to follow the DNR Order as long as it is valid and properly executed. |
| Public Awareness | California provides resources to educate the public about DNR Orders, ensuring that individuals understand their rights and options regarding end-of-life care. |
Dos and Don'ts
When filling out the California Do Not Resuscitate Order form, it is essential to approach the process thoughtfully. Here are some important dos and don'ts to keep in mind.
- Do ensure that you understand the implications of a Do Not Resuscitate Order.
- Do discuss your wishes with your healthcare provider and loved ones.
- Do fill out the form completely and accurately.
- Do sign and date the form in the presence of a witness if required.
- Do keep copies of the completed form for your records and share them with relevant parties.
- Don't use the form if you are unsure about your decision; seek guidance first.
- Don't leave any sections of the form blank; incomplete forms may not be honored.
- Don't assume that verbal instructions alone are sufficient; written documentation is crucial.
- Don't forget to review and update the form as your health or preferences change.
Similar forms
The Advance Healthcare Directive is a legal document that allows individuals to outline their preferences for medical treatment in the event they become unable to communicate their wishes. Similar to the California Do Not Resuscitate Order, it empowers individuals to make choices about their healthcare. This directive can include preferences regarding life-sustaining treatments, pain management, and organ donation. By designating a healthcare agent, individuals ensure that their medical decisions align with their values and desires, much like how a DNR specifies the desire not to receive resuscitation efforts.
The Physician Orders for Life-Sustaining Treatment (POLST) form is another document that shares similarities with the Do Not Resuscitate Order. POLST is designed for individuals with serious illnesses or advanced age who wish to convey their treatment preferences in a more detailed manner. This form goes beyond resuscitation preferences to include decisions about intubation, antibiotics, and other life-sustaining measures. Like the DNR, POLST is a medical order signed by a physician, making it actionable in emergency situations.
The USCIS I-864 form, which is essential in ensuring that immigrants receive the necessary financial support from their sponsors, aligns with various legal documents designed to protect individual rights and preferences in critical situations. For more information about the USCIS I-864 form, you can visit https://documentonline.org/blank-uscis-i-864.
The Living Will serves as a counterpart to the Do Not Resuscitate Order by outlining an individual’s wishes regarding end-of-life care. While the DNR focuses specifically on resuscitation efforts, the Living Will addresses broader medical treatment preferences. This document typically includes instructions about the use of life support and other interventions in situations where recovery is unlikely. Both documents aim to ensure that healthcare providers respect the patient’s wishes, even when the patient cannot voice them.
The Medical Power of Attorney (MPOA) is a legal document that grants a designated person the authority to make healthcare decisions on behalf of an individual. This document is similar to the Do Not Resuscitate Order in that it ensures the individual’s wishes are respected. While a DNR specifies a desire to avoid resuscitation, an MPOA can encompass a wider range of medical decisions. The agent appointed in the MPOA can advocate for the patient’s preferences, including those outlined in a DNR, ensuring a comprehensive approach to healthcare decisions.
The Do Not Intubate (DNI) order is closely related to the Do Not Resuscitate Order, but it specifically addresses the use of intubation during medical emergencies. While a DNR indicates that a patient does not wish to receive cardiopulmonary resuscitation, a DNI specifies that the patient does not want to be placed on a ventilator. Both documents reflect a patient’s preferences regarding life-sustaining interventions, and they work in tandem to provide clear guidance to healthcare providers about the individual’s wishes in critical situations.
Check out Popular Do Not Resuscitate Order Forms for Different States
Free Printable Dnr Form - A DNR Order’s presence can clarify intent during emergency medical situations.
Texas Dnr Form - Patients can change their DNR status at any time if their preferences change.
Polst Form Wa - Individuals must ensure they fully understand the potential outcomes before signing a DNR.
When dealing with traffic accidents in California, it's essential to understand the requirements for the CA DMV SR1 form, which must be submitted to the DMV for accidents involving personal injury, death, or significant property damage. Timely completion of this form is critical to maintaining your driving privileges, and if you're uncertain about the necessary documentation, you can refer to All California Forms for guidance.
Is a Dnr an Advance Directive - Helps avoid conflict between family members and medical staff.