Get Annual Physical Examination Form in PDF
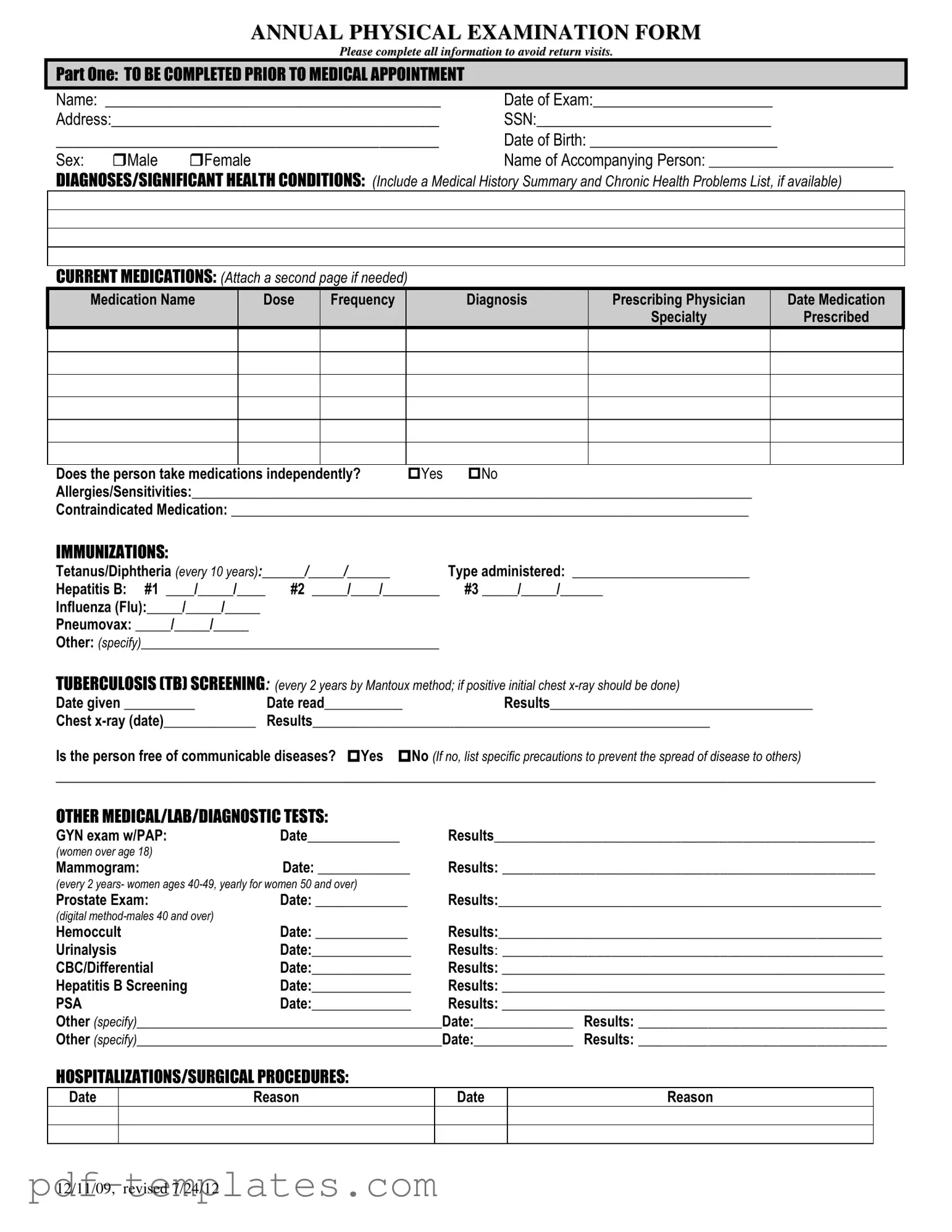
The Annual Physical Examination form serves as a crucial tool for individuals preparing for their yearly health check-up. This comprehensive document collects essential personal information, such as the patient's name, date of birth, and medical history, ensuring that healthcare providers have a complete picture of the patient's health. It includes sections for current medications, allergies, and significant health conditions, allowing for a thorough review of any ongoing treatments or concerns. The form also addresses immunizations, tuberculosis screening, and various medical tests, ensuring that patients are up-to-date with their health requirements. Additionally, it encompasses a general physical examination section that records vital signs and evaluates different body systems, enabling physicians to identify any potential issues. Finally, the form provides space for additional comments, recommendations for health maintenance, and any limitations or restrictions on activities. By completing this form accurately and thoroughly, patients can help streamline their medical appointments and enhance the quality of care they receive.
Misconceptions
Here are four common misconceptions about the Annual Physical Examination form:
- It is only for sick people. Many believe that an annual physical is only necessary if you are feeling unwell. In reality, this examination is important for everyone, regardless of current health status. It helps in early detection of potential health issues.
- Completing the form is optional. Some people think that filling out the form is not mandatory. However, providing complete and accurate information is crucial for the healthcare provider to assess your health properly and make informed recommendations.
- All questions are irrelevant. Individuals may feel that certain sections, like immunizations or medications, do not apply to them. Each question is designed to gather comprehensive health information, which aids in personalized care.
- Once completed, the form doesn't need to be updated. Many assume that the information provided remains valid indefinitely. In fact, it’s important to update the form regularly, especially after any changes in health status, medications, or allergies.
Annual Physical Examination: Usage Instruction
Completing the Annual Physical Examination form is essential for ensuring that all necessary health information is accurately recorded. After filling out the form, it will be submitted to your healthcare provider for review and further action. Please follow the steps below to fill out the form correctly.
- Begin with Part One. Fill in your Name and Date of Exam at the top of the form.
- Provide your Address and Social Security Number (SSN).
- Enter your Date of Birth and select your Sex by checking the appropriate box.
- Write the Name of Accompanying Person if applicable.
- List any Diagnoses or Significant Health Conditions. Include a summary of your medical history and any chronic health problems.
- Detail your Current Medications, including the name, dose, frequency, diagnosis, prescribing physician, and date prescribed. Attach an additional page if necessary.
- Indicate whether you take medications independently by checking Yes or No.
- List any Allergies/Sensitivities and any Contraindicated Medication.
- Complete the Immunizations section, filling in the dates and types for each vaccination.
- Fill out the Tuberculosis (TB) Screening section with the date given, date read, and results.
- Answer whether you are free of communicable diseases by checking Yes or No, and provide any necessary precautions if applicable.
- Document any Other Medical/Lab/Diagnostic Tests performed, including dates and results.
- List any Hospitalizations/Surgical Procedures with dates and reasons.
- Proceed to Part Two. Fill in your Blood Pressure, Pulse, Respirations, Temperature, Height, and Weight.
- Evaluate each system listed in the Evaluation of Systems section. Indicate normal findings and provide comments as necessary.
- Complete the Vision Screening and Hearing Screening sections, noting if further evaluation is recommended.
- Provide any Additional Comments regarding your medical history, medications, recommendations for health maintenance, and any special instructions.
- Indicate any limitations or restrictions for activities, checking No or Yes as applicable.
- Note if you use any adaptive equipment and if there has been a change in health status from the previous year.
- Complete the final sections regarding recommendations for care and specialty consults.
- Finally, ensure the Name of Physician, Physician’s Signature, Date, Physician Address, and Physician Phone Number are filled out accurately.
After completing all sections, review the form to ensure accuracy and completeness before submitting it to your healthcare provider.
Common mistakes
-
Incomplete Personal Information: Failing to fill out all personal details, such as name, date of birth, and address, can lead to delays. Ensure that all fields are completed accurately to avoid return visits.
-
Neglecting Medication Details: Omitting current medications or not providing the correct dosage and frequency can impact medical decisions. List all medications, including any changes since the last appointment.
-
Ignoring Allergies: Not disclosing allergies or sensitivities can pose serious health risks. It is essential to provide a complete list of any known allergies to prevent adverse reactions during treatment.
-
Missing Immunization Records: Failing to include immunization dates or not updating them can result in unnecessary vaccinations. Be sure to provide accurate and current immunization information.
-
Overlooking Health History: Not summarizing significant health conditions or past hospitalizations can lead to incomplete assessments. Include all relevant medical history to ensure comprehensive care.
File Specifics
| Fact Name | Description |
|---|---|
| Purpose of the Form | The Annual Physical Examination Form is designed to collect comprehensive health information prior to a medical appointment. It ensures that patients provide necessary details to avoid return visits. |
| Patient Information Required | Patients must complete personal information, including name, date of birth, address, and social security number. This data is essential for proper identification and record-keeping. |
| Immunization Records | Patients are required to provide their immunization history, including dates and types of vaccines received. This helps healthcare providers assess vaccination needs and health risks. |
| State-Specific Governing Laws | In some states, such as California, the use of this form is governed by the California Health and Safety Code Section 120875, which mandates health care providers to obtain comprehensive medical histories. |
Dos and Don'ts
When filling out the Annual Physical Examination form, it’s important to ensure accuracy and completeness. Here’s a list of things to do and avoid:
- Do fill in all required fields completely.
- Do provide accurate information about your medical history.
- Do list all current medications, including dosages and frequencies.
- Do mention any allergies or sensitivities clearly.
- Don't leave any sections blank; incomplete forms may lead to delays.
- Don't provide vague descriptions of health conditions; be specific.
- Don't forget to sign and date the form at the end.
- Don't rush through the form; take your time to ensure accuracy.
Similar forms
The Annual Physical Examination form shares similarities with the Patient Intake Form, commonly used in healthcare settings. Both documents require personal information such as name, date of birth, and contact details. They also gather medical history, including current medications and allergies. This information is crucial for healthcare providers to understand a patient's background and tailor their care accordingly. While the Patient Intake Form may focus more on initial visits, the Annual Physical Examination form emphasizes ongoing health assessments.
Another document similar to the Annual Physical Examination form is the Health History Questionnaire. This questionnaire delves into a patient’s past medical history, including surgeries, chronic illnesses, and family health history. Like the Annual Physical Examination form, it aims to provide a comprehensive overview of a patient’s health, ensuring that any potential issues are addressed during their visit. Both documents serve as tools for healthcare professionals to create effective treatment plans.
The Medication Reconciliation Form is also akin to the Annual Physical Examination form. Both documents track medications a patient is currently taking, including dosage and frequency. This is vital for preventing medication errors and ensuring that healthcare providers have an accurate understanding of a patient’s treatment regimen. The Annual Physical Examination form expands on this by including additional health information relevant to the patient’s overall wellness.
Similarly, the Immunization Record serves a comparable purpose. It documents a patient's vaccination history, which is a key component of preventive healthcare. The Annual Physical Examination form incorporates immunization details as part of a broader health assessment. Both documents highlight the importance of vaccinations in maintaining health and preventing disease outbreaks.
The Consent for Treatment form is another related document. It ensures that patients understand and agree to the medical procedures they will undergo. Like the Annual Physical Examination form, it emphasizes the importance of informed consent in healthcare. Both documents prioritize patient autonomy and the need for clear communication between patients and providers.
The Laboratory Test Request Form shares similarities with the Annual Physical Examination form, particularly in the context of diagnostic testing. Both documents may request lab tests based on a patient’s symptoms or health history. The Annual Physical Examination form may include lab test results, providing a more comprehensive view of the patient's health status, while the Laboratory Test Request Form focuses specifically on ordering tests.
The Referral Form is another document that aligns with the Annual Physical Examination form. It is used when a primary care provider refers a patient to a specialist for further evaluation or treatment. Both forms collect relevant patient information and medical history to ensure a smooth transition and continuity of care. The Annual Physical Examination form may indicate the need for referrals based on findings during the exam.
The Follow-Up Appointment Form is also comparable. This document is used to schedule subsequent visits based on the findings of an initial examination. Similar to the Annual Physical Examination form, it may include recommendations for further evaluation or treatment. Both forms play a critical role in managing ongoing patient care and ensuring that health issues are monitored over time.
The Advanced Care Planning Form is another relevant document. It addresses a patient’s preferences regarding future medical care and treatment options. While the Annual Physical Examination form primarily focuses on current health status, both documents encourage patients to think about their health goals and make informed decisions. This is particularly important for patients with chronic conditions or those nearing the end of life.
When considering financial management documents, the California General Power of Attorney form plays a crucial role by enabling an individual, known as the principal, to appoint an agent for financial decision-making. This form becomes particularly significant in circumstances where the principal is unable to oversee their financial affairs. It encompasses various powers related to financial management, from accessing bank accounts to navigating real estate transactions, making it an invaluable tool in stewardship. For more resources, you may refer to All California Forms that offer comprehensive templates and guidelines.
Finally, the Discharge Summary is similar to the Annual Physical Examination form in that it provides a comprehensive overview of a patient’s health status and care plan after a medical visit or hospitalization. Both documents summarize key findings, treatment recommendations, and follow-up care, ensuring that patients have a clear understanding of their health and what steps to take next.
Other PDF Forms
How to Calculate Electrical Load of a House in India - Support energy audits by providing necessary load documentation.
The Trader Joe's application form is a vital document for job seekers wishing to join this beloved grocery chain. It outlines necessary information about potential employees and provides an opportunity to showcase their unique skills and experience. For those interested, the application can be found at documentonline.org/blank-trader-joe-s-application/, and completing the form accurately can significantly increase the chances of landing a position at one of their stores.
Free Puppy Vaccine Record - Evidence of a dog's vaccination for public health purposes.